Legend One
Legend Two
Legend Three
Who should have tests for prostate cancer?
It is recommended that all men from the age of 50 have an annual digital rectal exam (DRE), and a PSA blood test. However, there are some men who have been found to be at a higher risk for developing prostate cancer.
Men who have a brother or father who have been diagnosed with prostate cancer have a 2 to 9 times higher risk of developing prostate cancer themselves. These men who are at high risk should have annual DRE exam and PSA from the age of 45.


What is the prostate gland and what does it do?
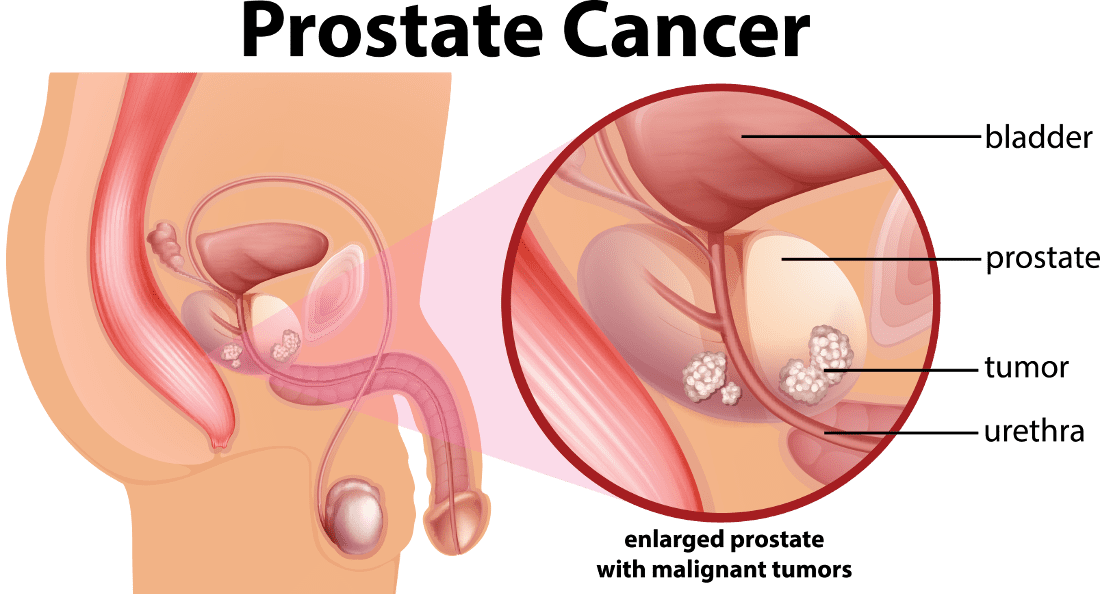
The prostate gland is normally the size of a walnut in the average adult male and will increase in size as men age. The urethra is the tube which delivers urine from the bladder through the prostate to the outside.
At the base of the bladder, the prostate gland surrounds the urethra. The prostate is an accessory part of the male ejaculatory system. Sperm are made and stored in the seminal vesicles until ejaculation occurs. The prostate gland provides 10-20% of the ejaculatory fluid. The precise function of the prostate is poorly understood. It is thought that its secretions may produce anti-bacterial substances to prevent urinary infection and possibly other secretions may play a role in fertilization. Nerves that control erection run alongside the gland, and may be carefully preserved in surgery to prevent impotence. This is called a nerve-sparing prostatectomy and is usually more successful in younger patients.
Prostate Cancer:
who’s at risk?
No one knows the exact causes of prostate cancer. Doctors cannot explain why one man develops the disease and another does not. Research has shown that men with certain risk factors are more likely than others to develop prostate cancer. (A risk factor is something that may increase the chance of developing a disease.)
Scientists have studied whether BPH, obesity, smoking, a sexually transmitted virus, or lack of exercise might increase the risk of prostate cancer. At this time, these do not appear to be important risk factors. Also, most studies have not found an increased risk of prostate cancer for men who have had a vasectomy (surgery to cut or tie off the tubes that carry sperm out of the testicles). Other possible risk factors are under study.
Many men who have known risk factors do not get prostate cancer. On the other hand, many who do get the disease have none of these risk factors. Men may want to talk with their doctor about factors that generally increase the chance of getting prostate cancer and about their own risk.
Studies have found the following risk factors for prostate cancer.

Risks factors
- Age: Age is the strongest risk factor for prostate cancer. This disease is rare in men younger than 45, but the chance of getting it goes up sharply as a man gets older. Most men with prostate cancer are older than 65.
- Family history: A man’s risk of prostate cancer is higher than average if his father or brother had the disease.
- Certain prostate changes: Having abnormal cells called high-grade prostatic intraepithelial neoplasia (PIN) may increase the risk of prostate cancer. These prostate cells look abnormal under a microscope.
- Diet: Some studies suggest that men who eat a diet high in animal fat or meat may be at increased risk of prostate cancer. Also, men who eat a diet rich in fruits and vegetables may have a lower risk.
Symptoms
Prostate cancer itself, when confined within the prostate gland, does not have any symptoms.
Urinary symptoms of an enlarged prostate, due to benign i.e. non-malignant growth, are very common. These include:
- Inability to urinate, or difficulty starting or stopping the urine flow.
- The need to urinate frequently, especially at night.
- Weak or interrupted flow of urine.
- Pain or burning during urination.
In most cases, these symptoms are not due to prostate cancer. They may be caused by benign enlargement of the prostate gland (benign prostatic hypertrophy – BPH), infection or inflammation, or another problem. However, a man with these symptoms should see a doctor so that any problem can be diagnosed and treated as early as possible. He may go to see his primary care doctor or a urologist, a doctor who specializes in diseases of the urinary system.
Common Questions
Q: I have urinary symptoms, should I be worried about prostate cancer
A: Symptoms of frequency, especially at night, urgency, stuttering of urine stream and waiting for urination increase with age. The most common cause is benign prostatic hypertrophy or BPH. This involves the benign enlargement of the prostate and is not associated with cancer. Treatment may start with oral medications to relax or shrink the prostate to improve the symptoms. Inflammation and infection of the prostate gland can also occur causing prostatitis, which will also cause urinary symptoms. Treatment for prostatitis is usually with a prolonged course of antibiotics. One should consult with their family physician to determine what the cause of symptoms may be.
Q: I have NO urinary symptoms, should I be worried about prostate cancer?
A: Prostate cancer does not usually cause urinary symptoms. The only means to identify prostate cancer early is a digital rectal exam and PSA. When symptoms are present in prostate cancer the disease is almost always advanced.
When can I return to sexual activity?
Let the surgery heal for three to four weeks before attempting anything. It is recommended you wait at least one month before you resume sexual activity.
Stimulation of the nerves is thought to be a first step on the journey back to potency. Remember that you can still experience the pleasures of orgasm and other sensual stimulations without full erections.
The average time to recovery for erections adequate for intercourse (in those who do recover) is 12-24 months, but in some men it is even longer.
I don’t have erections after surgery, am I impotent for life?
Think of your erections as a well conditioned athlete, who has been injured. This injury is going to take time to heal. You should try to remain patient, and remember that this will be an ongoing battle for many months and even years.
Rehabilitation of potency is much like a sports injury. Proper conditioning and medical treatment may potentially speed up recovery, but it is not guaranteed.
If you see any fullness in your erections in the months after surgery, this is a positive sign that some of the nerves are working or re-growing.
You are taking the first steps down the potency recovery path. Remember though, as shown in the previous table for open prostatectomy, 25-55% of men do not regain erections.

The Prostate
One in six Australian men will be diagnosed with prostate cancer within their lifetime, 12,000 are diagnosed each year. Approximately 2,600 Australian men die annually due to prostate cancer, making it the second most fatal cancer in men.
Advances in the early detection and treatment of this disease are believed to have sharply increased survival.
Survival Rates
Ten-year disease specific survival rates of patients with radical prostatectomies are greater than 90% for low grade adenocarcinomas, greater than 85% for medium grade adenocarcinomas.
When removal of the prostate is warranted, several important factors regarding the procedure are commonly taken into consideration by both patients and physicians:
- Cancer Removal
- Safety
- Continence
- Potency
The important thing is recovery.


The Latest Care
Professor Tony Costello makes use of Laparoscopic Prostatectomy assisted by the da Vinci Robotic System.
This groundbreaking technology, listed as number one in Forbes Magazine’s “Five Robots That Will Change Your Life,” provides unprecedented laparoscopic vision and precise robotic instrument manipulation.
This advanced technology is in the skilled hands of Professor Tony Costello. He is Australia’s first ever Professor of Urology and performs over 100 such procedures a year. He was the first to use the Robot in Australia.
Surgeons from around the world visit Professor Costello regularly to learn from his techniques.
Private Practice
Helen Crowe is an experienced urology nurse who has worked with Professor Costello in his private practice for over 10 years. Helen has developed expertise in educating and assisting patients and partners cope with the consequences of prostate cancer treatment.
For the past ten years Helen has convened the Nursing & Allied Health program of the annual Asia-Pacific Prostate Cancer Conference. This highly successful and highly regarded program attracts prostate cancer nurses, continence physiotherapists, psychologists and exercise physiologists to present and learn about best practise, multi-disciplinary care of men who have prostate cancer, and their partners.
Helen collaborates with Professor Costello to work closely with patients and their partners before surgery, whilst they are in hospital, and post-operatively. She is also responsible for follow-up and data collection for all patients who undergo robotic radical prostatectomy, so that Professor Costello has accurate feedback on the progress of all patients, including those who have travelled to Melbourne for treatment and who are attending their local specialists for follow-up management.
Helen has researched, published, presented and won awards for her work on quality of life issues related to prostate cancer treatment.


Epworth Hospital
Epworth Hospital provides expert urology nursing for patients admitted to the hospital. The nurses are involved in collecting quality care data on all patients undergoing robotic radical prostatectomy and have presented this work at state and national nursing forums.
Within the urology operating suite at Epworth Hospital are highly skilled and experienced anaesthetists, urology theatre nurses and theatre technicians. For robotic surgery to be successful, a team such as this is essential, and key members of the team underwent training in the USA to become familiar with all aspects of the robot setup and care. They are now responsible for providing this training for others both at Epworth Hospital and other centres.
Clinical Psychology
Several years ago Professor Costello realised the potential long-term impact of the diagnosis of prostate cancer on the quality of life of the patients, and also on their partners. In order to address this need, at Professor Costello’s request, The Royal Melbourne Hospital appointed the first clinical psychologist to be attached to a Urology Department in Australia.
The clinical psychologist appointed to the Urology Department accepts referrals to see both private patients and patients from within The Royal Melbourne Hospital. They provide counselling to assist patients dealing with the diagnosis of prostate cancer, making decisions about treatment options, coping with the post-operative problems of incontinence and erectile dysfunction. They see patients and their partners individually and together, and also run a support group for men with prostate cancer, providing the opportunity for men to gain support from others experiences, sharing common problems and solutions.


Working with me for over 20 years.
Helen has researched, published, presented and won awards for her work.
Travelling to Melbourne for Surgery
We have many patients travelling from interstate for their consultation with Professor Costello and their surgery.
Do I have to travel to Melbourne for an appointment with Professor Costello, and then travel again for my operation?
No, we can exchange a lot of information by phone, fax, email and mail, so that before you meet with Professor Costello we will have all of the information we need. We will also be able to make sure that you have all of the information that YOU need to be able to make a decision about whether or not you feel comfortable about coming to Melbourne for your surgery. We will be able to schedule an appointment for you with Professor Costello the day prior to your surgery to save you spending unnecessary time away from home.
How long would I have to be in Melbourne?
Usually patients need to be in Melbourne the morning prior to their scheduled surgery. You will have a urinary catheter, which will be removed by Helen Crowe one week after your operation. It is safest to remain in Melbourne for a day or two after this is removed, about 8-9 days following your operation. Then it should be perfectly safe to travel home. If you are travelling by plane, it is probably a good idea to have a transferable return flight home, in the highly unlikely event of something unpredictable causing a delay in you leaving Melbourne.
What if there are problems when I go home?
We keep an eye on all of our patients no matter how far away they are. If you have any problems or queries at all you are able to ring our rooms or email us at any time. We often can sort things out for you over the phone or with the help of your GP or local urologist. Very occasionally we will need you to return to Melbourne so that we can sort out a problem.

